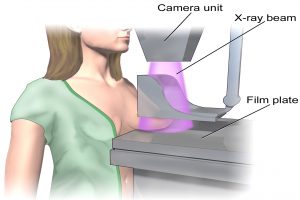
 Mammography is a technique that uses X-rays to provide an image of the breast. The image, called a mammogram, is used to find potential signs of breast cancer – such as tumors, small clusters of calcium (microcalcifications) and abnormal changes in the skin. A mammogram can detect a lesion when it is half the size of one that can be felt by touch. Mammography is the best screening tool available today for breast cancer. It can find cancers at an early stage, when they are small and most responsive to treatment.A typical mammogram consists of two views of each breast in which they are compressed firmly between two plates. The best time for breast examination is 5-7 days after cessation of menses, when the influences of hormones are minimal. This is also when, generally speaking, the breasts are less sensitive, therefore considered the most comfortable and least painful time to have a breast exam.The complete procedure takes only a few minutes, and is performed by a trained technologist under the supervision of our qualified radiologists. A physician analyzes the X-rays, looking for specific abnormalities or changes related to breast cancer. A written report is then sent to you and your doctor. On occasion, the physician may order additional views or other modalities, such as an ultrasound. In some cases, a doctor may also request follow-up consultation for ongoing diagnostic reasons – in which case, the physician will contact you directly to go over any details or assessments that she/he may have in addition to our reports. You stand in front of a special x-ray machine. The person who takes the x-rays, called a radiologic technician, places your breasts, one at a time, between an x-ray plate and a plastic plate. These plates are attached to the x-ray machine and compress the breasts to flatten them. This spreads the breast tissue out to obtain a clearer picture. You will feel pressure on your breast for a few seconds. It may cause you some discomfort; you might feel squeezed or pinched. This feeling only lasts for a few seconds, and the flatter your breast, the better the picture. Most often, two pictures are taken of each breast — one from the side and one from above. A screening mammogram takes about 20 minutes from start to finish. Screening mammograms are done for women who have no symptoms of breast cancer. It usually involves two x-rays of each breast. Screening mammograms can detect lumps or tumors that cannot be felt. They can also find microcalcifications or tiny deposits of calcium in the breast, which sometimes mean that breast cancer is present. Diagnostic mammograms are used to check for breast cancer after a lump or other symptom or sign of breast cancer has been found. Signs of breast cancer may include pain, thickened skin on the breast, nipple discharge, or a change in breast size or shape. This type of mammogram also can be used to find out more about breast changes found on a screening mammogram, or to view breast tissue that is hard to see on a screening mammogram. A diagnostic mammogram takes longer than a screening mammogram because it involves more x-rays in order to obtain views of the breast from several angles. The technician can magnify a problem area to make a more detailed picture, which helps the doctor make a correct diagnosis. Breast cancer is the most common cancer in women, with 75% of cases occurring in women older than 40. Early detection saves lives. The earlier breast cancer is detected, the easier and more successful the treatment. Detected early, breast cancer is more than 95% treatable. Grand Avenue Imaging supports the following steps to good breast health, recommended by Susan G. Komen for the Cure, and suggested by American Cancer Society: Annual Screening Mammography for women starting at age 40. Women under 40 with either a family history of breast cancer or other concerns about personal risk should consult with a trained medical professional about risk assessment and when to begin mammography. Clinical Breast Examinations by a trained medical professional at least every 3 years starting at age 20, and annually after 40 Monthly Breast Self-Examination (BSE) starting by age 20. Mammography is the best breast cancer screening method available today. It detects approximately 2-3 times as many “early” breast cancers as physical examination. Its key role is to identify a site of breast cancer early in its development when it is still very small, and often a year or two before a mass is large enough to be felt as a lump. In its early stages, breast cancers respond better to treatment, often requiring a much lesser degree of surgical or drug treatment. Very low doses of radiation are used during mammography screening. With advances in sensitivity and precision of radiological equipment, very low amounts of radiation are utilized to produce a very clear and precise image. Early detection is key, and mammography helps prevents the growth of a more prolific form of breast cancer. To prepare for a mammogram, you should dress comfortably in a two-piece outfit. (You will need to undress from the neck to the waist.) Please do not apply powders, deodorants or creams to your underarms or breasts – they may interfere with the clarity of an mammogram. For the purposes of accurate reporting, a radiologist requires high technical quality in each study. Interpreting mammograms takes considerable training and experience. In addition to strict federal compliance, Grand Avenue Imaging goes beyond the federal minimum requirements to deliver both early detection and peace of mind. Every exam is interpreted as follows: Category 0 Additional examination is recommended. If you are among the patients asked to return in six months for a special view of an area, your study is a Category 3. Our assessment of your examination is almost definitively negative, but there is a subtle area in question that we would appreciate re-examining in six months to insure its stability. This request is not a cause for alarm. It is simply a diagnostic follow-up in order to confirm our previous findings. The odds are upward of 90%that it is not a significant finding. However, it is only by being extremely careful and cautious with every subtle finding that we will discover, or uncover, the early preclinical and curable abnormalities for which we are constantly searching. If we request a six-month study, a letter will generally be sent to you and your referring physician explaining the reason for our request. The probability is high that this is not a significant finding. A personal reminder will be sent to you by your primary care provider at the time of the requested follow-up study. Only a limited study of the area in question will be necessary at that time. Women with implants require two additional views to visualize tissue. Using the Eklund Technique, implants are pushed back and breast tissue is pulled forward for evaluation. Q: What is a mammogram? A: A mammogram is an X-ray of the breast, and is the best screening tool widely available to detect breast cancer early. Q: Is a mammogram painful? A: During the procedure, each breast is compressed between two plates and an X-ray image is made. For some women, the pressure on the breasts can be uncomfortable and occasionally painful. Taking acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) about an hour before the exam can help make the experience more comfortable. Q: When is the best time to have a breast exam? A: The best time for breast examination is 5-7 days after cessation of menses. Generally speaking, the breasts are less sensitive, therefore the most comfortable and least painful time to have a breast examination. Q: How long does it take to perform a mammogram? A: The procedure usually takes about 10 minutes. Q: How do I prepare for a mammogram? What do I need to do the night before? A:To prepare for a mammogram, you should dress comfortably in a two-piece outfit. (You will need to undress from the neck to the waist.) Please do not apply powders, deodorants or creams to your underarms or breasts – they may interfere with the clarity of an X-ray. Q: How often should I get a mammogram? A: Starting at age 40, women should have annual screening mammograms. Women under age 40 with a family history of breast cancer and/or other concerns about their personal risk should consult with a healthcare provider about risk assessment and when to begin screening mammography. Q: Why are mammograms not recommended for women under 40? A: Mammography is a very effective breast cancer screening tool overall. However, it may be more effective at detecting tumors in older women than in younger women. Images on mammograms appear in gradations of black, gray and white, depending on the density of the tissue. Fat appears dark gray and cancerous tumors appear a lighter shade of gray or white. Unfortunately, dense normal breast tissue can also appear light gray on a mammogram, which can make mammograms harder to interpret in younger women, since they tend to have denser breasts. After menopause, though, breast density usually begins to decrease, making the mammograms of older women easier to read. Q: Does the radiation from a mammogram cause cancer? A: Today, mammography has little radiation risk. The amount of radiation that is used in mammography has been reduced greatly and is considered to be safe for women of the appropriate age. Q: How effective are mammograms? A: Mammography has the ability to detect breast cancers before they can be felt by touch. However, a small percentage of breast cancers cannot be identified by mammography. For this reason, it is important to follow the guidelines for clinical breast examination (CBE) and to practice monthly breast self-examination (BSE). Q: When is mammography not effective? A: Mammography may not help with a fast growing or aggressive cancer that has spread to other parts of the body prior to detection. Even though mammography can detect most tumors that are 5 millimeters in size, finding a small tumor does not always translate to early detection. Q: Why are breasts compressed during a mammogram? A: When the breasts are compressed the tissue is “spread out” and brought closer to the film, allowing for a sharply defined study. This is necessary in order to find the subtle underlying changes (or rule them out) vital to a complete, “highest quality” study. You are in charge. The technologists will ask you when the compression is reaching the point of discomfort. Please keep in mind, generally, the greater the compression, the more diagnostic the study. Q: What are calcifications? A: Calcifications are deposits of calcium that appear on a mammogram. In older women especially, calcium may leave the bones and appear in other parts of the body, such as the joints or breasts. But, clusters of tiny calcifications (microcalcifications) can be indications of precancer or cancer. Microcalcifications usually form as small, tight clusters in the ducts that can be seen on a mammogram. Although they are not themselves dangerous, they can be a warning sign of cancer and lead a doctor to perform follow-up tests to determine whether the area is cancerous or not. Q: Where can I get a free or low-cost mammogram? A: Contact your local Komen Affiliate, Health Department, Breast and Cervical Cancer Control Prevention (BCCCP) Program, YWCA’s EncorePlus Program and the American Cancer Society. Q: What is a “False Negative”? A: A false negative occurs when a mammogram appears “normal” even when breast cancer is present. False negatives are more common in younger women than in older women. The dense breasts of younger women contain many glands and ligaments that make breast cancers more difficult to identify in mammograms. As women age, breast tissue becomes more fatty and breast cancers are more easily seen by screening mammograms. Q: What is a “False Positive”? A: A false positive occurs when a mammogram is read as abnormal but cancer is not actually present. False positives are more common in younger women. For women of all ages, 5-10% of mammograms are abnormal and are followed up with additional testing (a diagnostic mammogram, fine needle aspirate, ultrasound or biopsy). Most abnormalities will turn out not to be cancer. |
